Background.
Clinical trials of mild cooling to 35°C or below in infants with early hypoxic–ischemic encephalopathy are under way. The objective of this study was to systematically document cardiovascular changes associated with mild therapeutic hypothermia and rewarming in such infants.
Patients and Methods.
Nine infants with gestational ages of 36 to 42 weeks, with 10-minute Apgar scores of 5 or less, clinical encephalopathy, and an abnormal electroencephalogram before 6 hours were cooled by surface cooling the trunk (n = 3) or by applying a cap perfused with cooled water (n = 6) for a median of 72 hours. The target core temperature was 34.0°C to 35.0°C for head-cooled infants and 33.0°C to 34.0°C for surface-cooled infants. Maintenance heating and rewarming were provided by an overhead heater.
Results.
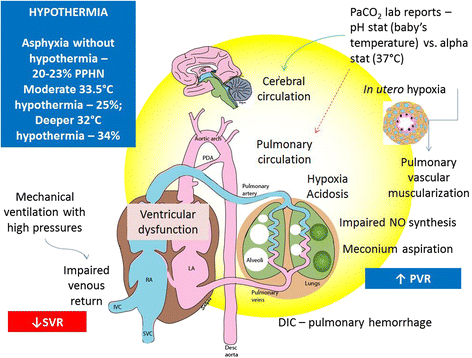
Mean arterial blood pressure increased by a median of 10 mm Hg during cooling and fell by a median of 8 mm Hg on rewarming. Heart rate decreased by a median of 34 beats/minute on cooling and increased by a median of 32 beats/minute on rewarming. A large increase in the output of the overhead heater decreased mean arterial blood pressure in 5 infants. Anticonvulsant drugs, sedatives, or intercurrent hypoxemia also produced falls in temperature. The inspired oxygen fraction had to be increased by a median of .14 to maintain oxygenation during cooling with 2 infants requiring 100% oxygen, an effect probably attributable to pulmonary hypertension, which was reversible with rewarming.
Conclusions.
Therapeutic cooling produces changes in heart rate and blood pressure that are not hazardous, but the combination of inadvertent overcooling and inappropriately rapid rewarming, together with sedative drugs that can impair normal thermoregulatory vasoconstriction, can cause hypotension in posthypoxic newborn infants.
Infants who already require 50% oxygen should be cooled cautiously because pulmonary hypertension may develop. Knowledge of these cardiovascular changes, careful monitoring, anticipation, and correction should help to avoid potential adverse effects in the upcoming clinical trials.








No comments:
Post a Comment